Wearable Health Sensors
MyA: Multi-Biometric Vest for People Living with Angelman Syndrome
Angelman syndrome (AS) is a neurogenetic syndrome associated with severe developmental and intellectual disability. Symptoms of AS include very limited speech, difficulty sleeping, and poor motor function. AS is caused by a mutation or deletion of the UBE3A gene on the maternal chromosome 15 and is typically diagnosed in the early childhood period using genetic testing. At present, there is no cure for AS. Treatment is focused on supportive therapies and pharmaceuticals to manage seizures and reduce behavior problems. The AS community is motivated to find a cure, and several major gene therapy trials are underway to reduce or potentially reverse symptoms.
Despite increased investment in clinical trials, functional outcomes that impact the lives of people living with AS and their families remain widely variable. A major barrier to clinical trials is the lack of available outcome measures suitable for AS. Wearable devices that monitor physiological and behavioral output are promising solutions because they provide objective metrics of physiological function without requiring verbal or motoric input from the patient. However, typical wearable devices in form factors such as smartwatches and headbands are often not tolerable by AS patients. Using input from AS caregivers from extensive focus groups (N = 8) conducted by our research team, we have designed MyA, a biometric vest that will measure several key signals relevant to AS (heart rate, respiration, vocalizations, temperature, and sleep), while meeting the unique sensory and tactile needs of the AS population. For our preliminary developments, we sewed conductive fabric and conductive silicone into separate commercially available athletic vests composed of primarily nylon, polyester, or polyamide. Our preliminary measurements of the electrocardiogram demonstrate the ability to capture key biosignals using our textile prototype. We were able to measure heart rate from the electrocardiogram within 2.4 beats per minute of a commercially available reference chest strap heart rate monitor with high correlation between the two devices (r = 0.88, p < 0.05).
For the proposed project, the Protégé Scholar will work closely with a senior member of the lab to integrate additional sensors into the prototype. The sensors will include but are not limited to, audio, GPS, locomotion, skin temperature, ambient temperature, ambient humidity, and Bluetooth Low-Energy. The Protégé Scholar will work with the senior member of the lab to validate each sensor on the benchtop and develop code that can be integrated seamlessly into the biosensor prototype.
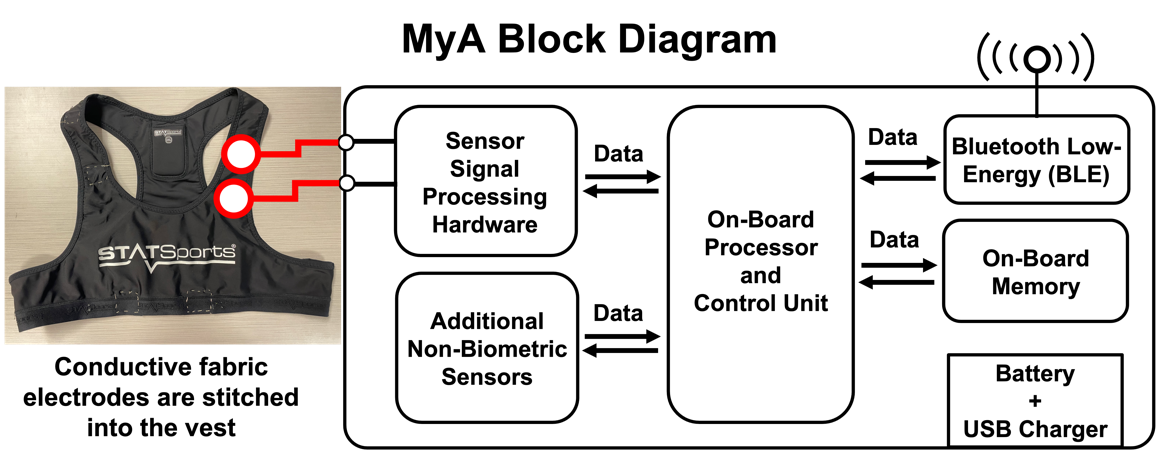
Figure 1. MyA system block diagram depicting essential internal functions as well as connections to the textile.
Project 2: Smart Helmets for Detecting and Preventing Concussions

Figure 1: The first smart helmet used an array of rosette strain gages to measure the deformations of the helmet shell during impact and analytical models related those strains to the impact force. We are currently developing a second-generation system to determine the placements for the minimum number of sensors required to reconstruct impacts over the entire surface of the helmet.
We are all familiar with the sight of an athlete experiencing a severe blow to the head and being unable to stand or walking shakily back to the sideline. In those instances, it is clear that the athlete has experienced a “concussion.” Concussion, as defined by the Guideline Development Subcommittee of the American Academy of Neurology, is a syndrome of biomechanically induced alteration of brain function potentially affecting memory, orientation, and state of consciousness and is the most common type of mild traumatic brain injury. Despite early work suggesting that concussion symptoms were directly correlated with the magnitudes of singular impacts, a more complete analysis of the data has made it clear that an impact threshold does not exist. In fact, the deleterious consequences of repetitive head impacts or sub-concussive blows can accumulate over time, causing tissue level damage that both increases susceptibility to later head impacts, and generally increases the volume of damaged brain tissue.
While numerous attempts have been made to design sensor systems to measure head impacts, including in-helmet systems, wearable accelerometers, and even mouthguards, they only quantify risk of injury and even so with varying accuracy. Additionally, these sensors do little to encourage better technique. Recent work demonstrating that improved technique decreases an athlete’s exposure to head impacts suggests that the best intervention is one that helps coaches better prepare their athletes for practices and games. The goal of this project is to develop a system that mitigates head injury by tracking the force of each hit and provides a video-based tool that will allow coaches to teach better technique.
The Protégé Scholar will work with a senior member of the Hoilett and Human Injury Research and Regenerative Technologies (HIRRT) labs to develop a miniaturized device that combines high impact accelerometers, GPS, and Bluetooth capabilities into a single, discreet wearable. The wearable will track the force delivered by repetitive head impacts, map the location of these forces in real-time on a practice field, and relay this information back to a bay station that can be monitored by coaches and athletic training staff.
Project 3: NeoWarm: Kangaroo Mother Care with Integrated Thermal Management and Vital Signs Monitoring
Neonatal hypothermia is one of the most common and dangerous complications of premature birth. In resource-rich settings, incubators are typically used to prevent hypothermia; however, incubators are scarce in low/middle-income countries (LMICs). Kangaroo Mother Care (KMC) is a technique that effectively combats the lack of incubators in LMICs. In KMC, a caregiver holds the newborn to their bare chest, augmenting the newborn’s compromised thermoregulation system. While KMC is highly effective, it requires the participation of the caregiver at all times and poses challenges for vitals monitoring used to assess the newborn’s health during their early stages of life. As a response to this need, we have developed NeoWarm, a device that will augment KMC. NeoWarm is an insulated newborn carrier with integrated sensors for monitoring temperature, heart rate (HR), respiratory rate (RR), and particularly, blood-oxygen (SpO2) to detect apnea, another common complication of premature birth. Additionally, when the caregiver needs a break to care for themselves, NeoWarm can function as a stand-alone unit, monitoring and maintaining the newborn’s temperature without the caregiver.
The Protégé Scholar will work with a senior member of the lab to integrate each sensor into a single device. The scholar will help develop a professional-grade printed circuit board as well as firmware that will simultaneously track each physiological signal of interest using a microcontroller and send the resulting data to a previously developed smartphone application using Bluetooth Low-Energy.
Director

Orlando Sanguinette Hoilett
Asst Professor, CEAS - Biomedical Eng
501 MANTEI